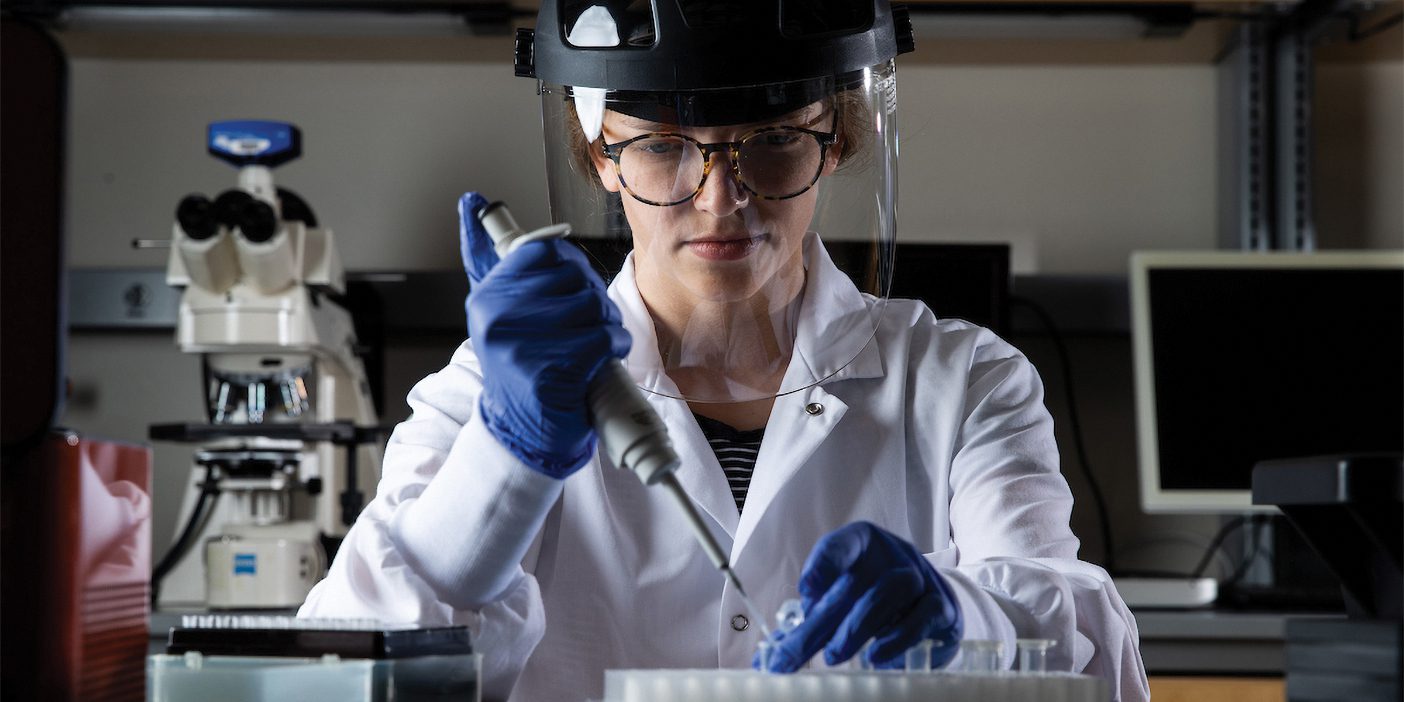
Microbiology and molecular biology professor Brett E. Pickett (BS ’05) has spent his career studying viruses, from common influenza to Zika. When SARS-CoV-2 (aka COVID-19) began spreading in Wuhan, China, he set his research aside and pulled 12–15 hour days to help the scientific community unpack this new coronavirus. Here he fields questions on virology and how his work is adding to the world’s understanding of COVID-19.
How many viruses are out there?
Probably millions, but some affect only bacteria, animals, or plants. As humans, we have to worry about a few hundred.
What are the signatures of the big viruses you’ve studied?
For the flu, its ability to change every year. Sometimes we can anticipate how it will change, but not always. For Zika, its genome changes relatively often, but it is able to infect only certain cell types, mostly brains. That and Zika can make copies of itself in both a mosquito and in a human. For SARS Coronavirus 2, its signature is still being determined, but it’s a virus that can cause havoc in a lot of different cell types. Many viruses, like the flu, can get into only a few types of cells. However, this coronavirus gets into lung, heart, gut, and kidney cells.
What research are you doing to help understand COVID-19?
I research how human cells react and change as they’re infected with the virus and which genes we can potentially turn on and off to help fight it.
As viruses go, how scary is COVID-19?
Since 2000 or so, there have been local or global epidemics every few years. There are scarier viruses out there that kill 50 to 80 percent of those who get them. The current COVID-19 death rate is relatively low—there’s just been a lot of people who have been exposed to it so the numbers seem to be higher than we’re used to seeing from past instances of small outbreaks with very dangerous viruses.
What gives you hope right now?
Tools and processes developed in the last 15 years help us make progress quickly: from electron-microscope pictures of a virus to sequencing its genome to figuring out how humans respond to a virus to quickly interpreting the results of experiments. Combining these tools with the relatively low death rate, we’ll get through this.